Each of these appendices and supplementary documents was less thoroughly edited than Sentience Institute’s usual standard, in order to reduce the time required to summarize the extensive health behavior literature. The main report is available at: http://sentienceinstitute.org/health-behavior
Table of Contents
Theory of reasoned action/theory of planned behavior The health action process approach Empirical testing of social cognition models Usefulness of social cognition models |
Several theories and models have been proposed about what affects intentions to modify health behaviors. These can be referred to as “social cognition models” (SCMs). These SCMs are frequently used as the basis for designing health behavior interventions, though it is unclear whether they encourage substantial changes in the design in practice. Some of the factors identified as important determinants of health behavior may also determine behavior relevant to the farmed animal movement and other social movements. SCMs do not cover all possible determinants of intentions and behavior, usually excluding neurobiological, cultural, demographic, and personality factors. Nevertheless, an understanding of these SCMs may help to inspire new approaches in designing interventions or new avenues for research in the farmed animal movement.
The health belief model
The health belief model (HBM) emphasizes that in order for someone to take action to avoid ill-health or improve their health, they would need to believe:
- “that he was personally susceptible to it,
- that the occurrence of the disease would have at least moderate severity on some component of his life,
- that taking a particular action would in fact be beneficial by reducing his susceptibility to the condition or, if the disease occurred, by reducing its severity, and that it would not entail overcoming important psychological barriers such as cost, convenience, pain, embarrassment,”[1] (which are sometimes separated into “benefits” and “barriers”).
Additionally, though not included as a factor in the original conception of the HBM, “[a] factor that serves as a cue, or a trigger, to appropriate action appeared to be necessary.”[2] Cues to action have not been well-studied in the context of the HBM.[3] Later, individual motivation and individual self-efficacy (one’s perception of their ability to successfully perform a behavior) were also added to the HBM, but have not been well-studied in this context.[4]
There are other limitations to the applicability of the HBM. It may be better at representing past decisions than predicting future behavior, for example.[5]
Protection motivation theory
Protection motivation theory (PMT) suggests that people protect themselves based on their perceptions of:
- “The noxiousness or severity of the threatened event,”
- “The probability of the occurrence of the event,”
- “The efficacy of a recommended coping response,” and
- “Self-efficacy.”[6]
Note that this parallels the criteria of the HBM, except that self-efficacy (which was only subsequently added to the HBM) is viewed as a core component and that psychological barriers are not accounted for in PMT.
The transtheoretical model
The transtheoretical model (TTM) “posits that individuals progress through five stages of change on their way toward adopting a healthy behavior or toward cessation of an unhealthy behavior”:
- “precontemplation (not intending to change),
- contemplation (intending to change in the foreseeable future),
- preparation (planning to change very soon and currently taking measurable steps to change),
- action (changed in the past 6 months), and
- maintenance (changed and sustained the behavior change for 6 months or more).”
Additionally, the TTM “describes the change process as cyclical rather than linear, as individuals may move forward through stages, backslide, and then continue cycling and recycling through the stages of change.”[7]
One paper argues that the TTM “is very versatile and can be easily used to describe the process of change that a person goes through to become vegan.”[8]
Self-determination theory
Self-determination theory (SDT) is a macro theory on human motivation, which has been applied to understanding health behavior. SDT examines how extrinsic forces interact with intrinsic motives and needs. Its proponents emphasize internal motivations and a natural tendency for humans towards personal development, but allow a role for conditions that support or hinder an individual’s needs of “autonomy, competence, and relatedness.”[9] They argue that social context can either help or hinder an individual through its effect on these three needs.[10]
Theory of reasoned action/theory of planned behavior
The theory of reasoned action (TRA) is a theory of human behavior that explains behavior as being a result of individuals’ intentions. These intentions are in turn shaped by:
- “subjective norms” and
- “attitudes towards the behavior.”[11]
The theory of planned behavior (TPB) extends TRA, adding an extra predictor of intentions:
- “perceived behavioral control,” which is similar to self-efficacy, comprising “judgments of how well one can execute courses of action required to deal with prospective situations.”[12]
Prototype-willingness model
The prototype-willingness model (PWM) was developed out of the TRA/TPB to account for behavior not well-explained by existing SCMs.[13] As well as a “reasoned pathway” to health or risk behaviors, it suggests a “social reaction pathway.” The social reaction pathway includes four factors that affect individuals’ willingness to engage in risk behaviors when they are in risk-conducive situations:
- Subjective norms,
- Attitudes,
- Past behaviors, and
- The prototype: “the image that people have of the type of person who engages in a particular behaviour.”[14]
Social cognitive theory
Social cognitive theory (SCT) is a theory of learning that suggests that people learn through “direct” and “observational experience,” and that this leads them to reproduce certain behaviors. This is influenced by three “interacting determinants that influence each other bidirectionally”:
- “Personal factors in the form of cognitive, affective, and biological events,,
- Behavioral patterns, and
- Environmental events.”[15]
The health action process approach
The health action process approach (HAPA) emphasizes three stages of influence on health behavior decisions:
- Pre-intenders: “the influences on deciding whether to change one’s behaviour,”
- Intenders: “the influences on deciding how to act in support of the decision to change,”
- Actors: “the influences on acting and continuing to act.”[16]
Empirical testing of social cognition models
SCMs have been empirically tested for their accuracy in describing and predicting behavior change, though they arguably do not make meaningful predictions.
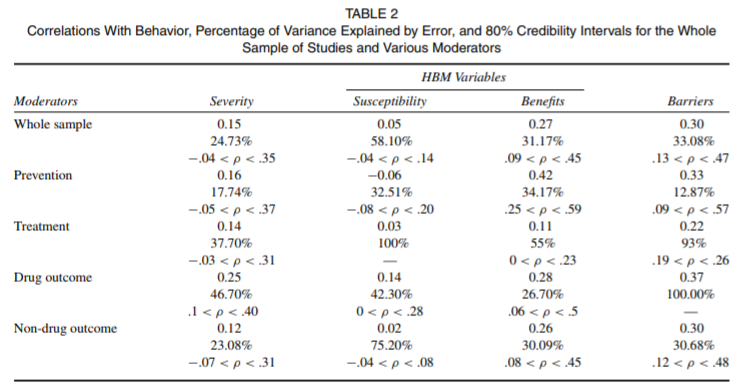
For example, a meta-analysis of 18 studies determined the correlations between survey questions designed to capture aspects of the HBM (severity, susceptibility, benefits, and barriers) with measurements of the target behavior in each study. It found a small effect for “severity,” a “near zero” effect from “susceptibility,” a small effect from “benefits,” and a medium (reverse-coded) effect from “barriers.”[17]
Fig. 1. Correlations between aspects of the health belief model and behavior.
In this meta-analysis, in several ways “barriers” appears to be the strongest predictor in the HBM; it had the largest effect size (r = 0.30), homogenous results, and a much smaller correlation between the length of time between the measurement of attitudes and the decision over the behavior adopted than the other predictors (r = 0.02, compared to -0.37, 0.50 and 0.59). Both “benefits” and “barriers” had small effect sizes in contexts attempting to treat cases of poor health, as opposed to preventing possible future instances.[18]
Another review found that, “success of intervention on adherence was unrelated to the HBM constructs addressed,”[19] which fails to support the conclusion of the above meta-analysis that perceived “benefits” and “barriers” were the strongest predictors of behavior.[20]
Broadly speaking, research has not shown any SCM to be consistently superior to the others. Psychologists Mark Conner and Paul Norman note that, “there is little consensus on whether some variables are more influential than others and whether some models of health behaviour are more predictive than others.”[21] Summarizing the existing comparisons between different SCMs and different predictors of intentions, they note that:
- “Early studies” comparing the HBM to TRA found little difference, or see one or the other as slightly better for particular issues. For example, “Hill et al. (1985) found the two models to explain similar amounts of variance in women’s intentions to perform breast self-examination (17-20% of variance) and to have a Pap test/cervical smear (26-32% of variance).” More recent studies reported the TPB to have greater predictive power than the HBM.[22]
- Several comparisons have found self-efficacy to be the most important, or second-most important, predictor of intentions and behavior.[23]
- “Other comparison studies have generally reported similar levels of predictive power for the SCMs examined.”[24]
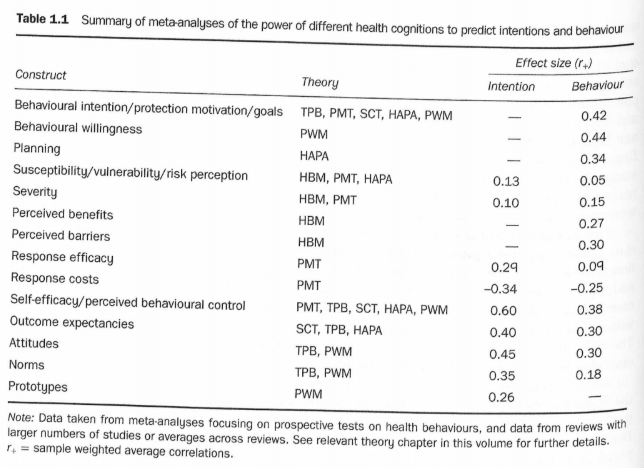
Combining the results of several meta analyses, Conner and Norman list the effect sizes of various predictors on intentions and on behaviors:[25]
Fig. 2. The effect sizes of various predictors on intentions and on behaviors.
This also gives us an idea of the differences between effect sizes on behaviors and intentions. For those constructs in the table above with effect sizes for both intentions and behavior, the effect on behavior averages 69% of the effect on intention. Conner and Norman add that, “Webb and Sheeran (2006) reviewed studies that significantly changed intentions (d+ = 0.66) and reported that these studies had medium-sized effects on behaviour (d+ = 0.36),”[26] which would be 55% of the effect for intentions. A meta-analysis of 204 experimental studies found effects on behavior from “[e]xperimentally induced changes in attitudes, norms, and self-efficacy” that were 79%, 74%, and 92% of the effect that these types of changes had on intentions.[27] These figures provide rough guides for the amount of behavior change we could expect to see if we successfully alter individuals’ intentions. A meta-analysis focused specifically on the TPB's application to understand and predict nutrition-related behaviors in youth found a moderate correlation between intention and behavior (r = 0.38).[28]
Conner and Norman warn that, “[r]eliability [i.e. correlation] of measures of intentions, self-efficacy, and other health conditions rarely exceed 0.80, meaning they contain less than 64% meaningful variance.”[29] When compared to interventions targeted at animal product consumption, contextual differences will render such figures even less accurate, so we should not place much weight on these precise figures for our purposes.
Usefulness of social cognition models
SCM theories have been used by some—but certainly not all—researchers in designing health behavior interventions.[30] Evidence that interventions that are guided by SCMs are more successful than those that are not is weak and inconsistent. Some reviews suggest no strong correlation or a negative correlation between SCM use and intervention effectiveness:
- Rhodes et al.’s overview of Physical Activity (PA) interventions,[31] a subsequent review of 171 PA studies,[32] and two reviews of digital interventions for reducing alcohol use found no strong effect from the explicit use of theory.[33]
- A meta-analysis of 190 interventions found that, “[i]nterventions based on Social Cognitive Theory or the Transtheoretical Model were similarly effective and no more effective than interventions not reporting a theory base.”[34]
- One meta-analysis of text message studies even found that, “[i]nterventions with no apparent theoretic foundation had a larger effect (d=0.37, 95% CI 0.25, 0.48) than those reported to be guided by specific theoretic models (d=0.19, 95% CI 0.11, 0.27).”[35]
In other cases, however, the findings are more positive:
- One overview found that, “[a]ll theory-informed interventions (10 of 40 studies) showed significant improvements in diet quality,” though “direct associations” were not established.[36]
- A review of the influence of behavioral theory on fruit and vegetable intervention effectiveness among children found that, “[p]redicating an intervention on behavioral theory had a small to moderate enhancement (P < .001) of outcome effectiveness.”[37]
- An overview of behavioral HIV-prevention interventions for adolescents noted that three out of five included meta-analyses “found a positive association between theory-based interventions and efficacy, and the others did not consider this factor directly. All of the [six] qualitative reviews considered this factor and concluded it was associated with intervention success.”[38]
- In one overview, 4 of 17 included reviews “reported positive associations between theory-based interventions and short term PA uptake.”[39]
- In one review, “[t]he only intervention feature in the moderator analysis that was associated with clinically significant reductions in HbA1c was the “use of theory/model” to inform interventions.”[40]
- In another review, the authors found that, “[i]nterventions explicitly targeting behavioural determinants from the theory of planned behaviour (including reasoned action approach and health action process approach models) or social-cognitive theory produced greater effect sizes on [motivation as measured by the theories of] intention and stage of change than studies which did not target these constructs.”[41]
Conner and Norman identify seven areas of overlap between the SCMs.[42] Combined models have therefore been proposed,[43] although these combined models are still open to criticism.[44]
Given the inconsistency with which use of SCMs in intervention design is associated with greater intervention effectiveness, it may not be worth the resource cost for researchers in the farmed animal movement to develop animal product consumption-specific behavior change theories or to utilize existing SCMs. Nevertheless, the farmed animal movement may benefit from using existing SCMs in moderation to inspire variations in intervention design that can be tested for their effectiveness.
[1] Irwin Rosenstock, “Historical Origins of the Health Belief Model,” Health Education & Behavior 2, no. 4 (1974), 330, describing “The earliest characteristics of the Model.”
[2] Irwin Rosenstock, “Historical Origins of the Health Belief Model,” Health Education & Behavior 2, no. 4 (1974), 332.
[3] Christopher J. Carpenter, “A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior,” Health Communication 25, no. 8 (December 2010), 662, notes that, “Rosenstock and every other reviewer of the literature since his initial work have noted that the cue to action is the most underdeveloped and rarely measured or researched element of the model (Janz & Becker, 1984; Rosenstock, 1974; Zimmerman & Vernberg, 1994). While the cue to action may be important, it is not examined in the current review, as there are not enough studies that measured it.”
Christina Jane Jones, Helen Smith, and Carrie Llewellyn, “Evaluating the effectiveness of health belief model interventions in improving adherence: a systematic review,” Health Psychology Review 8, no. 3 (2013), 264, note that, “[o]ur review corroborated the finding that the cues to action construct is the most rarely measured (Carpenter, 2010; Zimmerman & Vernberg, 1994).”
[4] Christopher J. Carpenter, “A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior,” Health Communication 25, no. 8 (December 2010), 662 notes that, “Becker (1974) proposed that overall motivation to pursue healthy behavior should be included. Self-efficacy was also proposed as an HBM variable (Rosenstock, Strecher, & Becker, 1988). However, these variables are rarely included in HBM studies (Zimmerman & Vernberg, 1994), which precludes quantitative summary. Furthermore, Zimmerman and Vernberg questioned whether or not the HBM is still the same model when these other variables are added.”
[5] Christopher J. Carpenter, “A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior,” Health Communication 25, no. 8 (December 2010), 663, summarizing the contributions of previous meta-analyses, notes that, “[t]he most complete meta-analysis was conducted by Harrison et al. (1992). The Harrison et al. meta-analysis concluded that retrospective studies produced substantially larger effect sizes than prospective studies. This suggests that the HBM is not as good at predicting future behavior as its creators had hoped. The estimates of the effect of each variable on behavior were all fairly small in their meta-analysis.”
[6] James E. Maddux and Ronald W. Rogers, “Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change,” Journal of Experimental Social Psychology 19, no. 5 (September 1983), 470. They note that some of their original formulations of PMT did not include self-efficacy, but on 476 they conclude from their experiment that, “[n]ot only did self-efficacy expectancy significantly influence intentions to adopt the recommended coping behavior, but self-efficacy expectancy proved to be the most powerful predictor of behavioral intentions.”
[7] Seth M. Noar, Melissa S. Harris, and Christina Anderson, “Does Tailoring Matter? Meta-Analytic Review of Tailored Print Health Behavior Change Interventions,” Psychological Bulletin 133, no. 4 (August 2007), 674, citing J. O. Prochaska and C. C. DiClemente, “Stages and processes of self-change of smoking: Toward an integrative model of change,” Journal of Consulting and Clinical Psychology 51 (1983), 390-5 and J. O. Prochaska, C. C. DiClemente, and J. C. Norcross, “In search of how people change: Applications to addictive behaviors,” American Psychologist 47 (1992), 1102-14.
[8] Elisabeth Mendes, “An Application of the Transtheoretical Model to Becoming Vegan,” Social Work in Public Health 28, no. 2 (2013), 142-9.
[9] Richard M. Ryan and Edward L. Deci, “An overview of self-determination theory: An organismic-dialectical perspective,” in Edward L. Deci and Richard M. Ryan (eds.) Handbook of Self-Determination Research (New York, NY: University of Rochester Press, 2002), 5 note that SDT recognizes “that there is compelling evidence in favor of human tendencies toward active engagement and development” but also that there is “manifold indication of fragmentation and conditioned responses,” and “provides a framework that integrates the phenomena illuminated by these discrepant viewpoints.” This is important because, “[i]nsofar as practitioners believe people have a natural tendency toward gaining integrity and enhancing their human potentials, they will orient to supporting and facilitating that endogenous tendence across a variety of settings, including homes, schools, work organizations, and therapy clinics. In contrast, insofar as practitioners assume no such inner tendency toward growth, self-construction, and inner coherence, then educational, therapeutic, and other practical intervention strategies will focus on exogenous means of training, shaping, controlling, and directing behavior towards ends deemed to be of value.”
On pages 7-8, they summarize that, “[c]ompetence refers to feeling effective in one’s ongoing interactions with the social environment and experiencing opportunities to exercise and express one’s capacities… Relatedness refers to feeling connected to others, to caring for and being cared for by those others, to having a sense of belongingness both with other individuals and with one’s community… autonomy refers to being the perceived origin or source of one’s own behavior… one can quite autonomously enact values and behaviors that others have requested or forwarded, provided that one congruently endorses them.”
[10] Richard M. Ryan and Edward L. Deci, “An overview of self-determination theory: An organismic-dialectical perspective,” in Edward L. Deci and Richard M. Ryan (eds.) Handbook of Self-Determination Research (New York, NY: University of Rochester Press, 2002), 9 note that, “[t]o the extent that an aspect of the social context allows need fulfillment, it yields engagement, mastery, and synthesis; whereas, to the extent that it thwarts need fulfillment, it diminishes the individual’s motivation, growth, integrity, and well-being.”
[11] Icek Ajzen, “The theory of planned behavior,” Organizational Behavior and Human Decision Processes 50 no. 2 (December 1991), 179.
[12] Icek Ajzen, “The theory of planned behavior,” Organizational Behavior and Human Decision Processes 50 no. 2 (December 1991), 183-4.
[13] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 13.
[14] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 13. Note that these authors are summarizing the theory, they are not the original proponents.
[15] Albert Bandura, “Social Cognitive Theory of Mass Communication,” Media Psychology 3, no. 3 (2001), 265-6.
[16] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 14. Note that these authors are summarizing the HAPA, they are not the original proponents.
[17] Christopher J. Carpenter, “A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior,” Health Communication 25, no. 8 (December 2010), 661-669. Note the wide range of p-values in the reported results, and that the results of “susceptibility” and “benefits” were described as heterogeneous by Carpenter. Judged by the AMSTAR 2 criteria, the meta-analysis warrants only “critically low” confidence in its results.
[18] Christopher J. Carpenter, “A Meta-Analysis of the Effectiveness of Health Belief Model Variables in Predicting Behavior,” Health Communication 25, no. 8 (December 2010), 661-669.
[19] Christina Jane Jones, Helen Smith, and Carrie Llewellyn, “Evaluating the effectiveness of health belief model interventions in improving adherence: a systematic review,” Health Psychology Review 8, no. 3 (2013), 264.
[20] Christina Jane Jones, Helen Smith, and Carrie Llewellyn, “Evaluating the effectiveness of health belief model interventions in improving adherence: a systematic review,” Health Psychology Review 8, no. 3 (2013), 265, suggests that “The fact that Carpenter’s (2010) meta-analysis included any health behaviour and this systematic review focused on adherence behaviour only, might account in part for the differing conclusions. A further explanation for the difference in findings could relate to the way the constructs are defined and measured, and how the model is operationalised. A minority of studies (5/18) reported measuring health beliefs related to the components found in the HBM pre-and post-intervention.”
On AMSTAR 2 criteria, the review was rated as warranting “moderate” to “low” confidence, depending on which domains are seen as critical. The authors note that, “the majority of studies failed to provide sufficient information to accurately assess risk of bias.”
266, notes that “The methodological quality of the studies was variable with recent studies more likely to demonstrate lower risk of bias compared to studies published in the 1990s and earlier,” that there is a “risk of positive publication bias,” and that, “[t]hree out of the 18 studies used the HBM in its entirety, and only five studies measured model constructs pre-and post-intervention. Only one study offered mediation analysis of HBM constructs on adherence behaviour. Overall, evidence for endorsing the model for use in adherence-enhancing interventions is weak, with no consistent relationship between HBM construct addressed and intervention success.”
[21] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 16. They add that, “[c]omparatively little empirical work has directly compared the predictive power of the different models (Noar and Zimmerman 2005; Glanz and Bishop 2010).”
[22] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 16.
[23] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 17 note that, “[t]wo comparison studies have focused on self-efficacy in relation to the main SCMs. Seydel et al. (1990) compared the HBM (i.e. susceptibility, severity, outcome expectancies) with protection motivation theory (PMT; i.e. susceptibility, severity, outcome expectancies, self-efficacy) and reported the outcome expectancies and self-efficacy to be the most important predictors of cancer-related preventive intentions and behaviour. Dzewaltowski (1989) compared the TRA, with self-efficacy emerging as the most important single predictor.”
[24] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 17.
[25] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 17. Note that they don’t discuss which meta analyses produced which results, or what methodology they used to combine the results.
[26] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 18.
[27] Paschal Sheeran, Maki Alexander, Erika Montanaro, Aya Avishai-Yitshak, Angela Bryan, William M. P. Klein, Eleanor Miles, Alexander J. Rothman, “The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis,” Health Psychology 35, no. 11 (2016), 1178-1188 summarize that, “[e]xperimentally induced changes in attitudes, norms, and self-efficacy all led to medium-sized changes in intention (d+ = .48, .49, and .51, respectively), and engendered small to medium-sized changes in behavior (attitudes-d+ = .38, norms-d+ = .36, self-efficacy-d+ = .47). These effect sizes generally were not qualified by the moderator variables examined (e.g., study quality, theoretical basis of the intervention, methodological characteristics, and features of the targeted behavior), although effects were larger for interventions designed to increase (vs. decrease) behavioral performance.”
[28] Shaun K. Riebla, Paul A. Estabrooks, Julie C. Dunsmore, Jyoti Savla, Madlyn I. Frisard, Andrea M. Dietrich, Yiming Peng, Xiang Zhang, and Brenda M. Davy, “A systematic literature review and meta-analysis: The Theory of Planned Behavior's application to understand and predict nutrition-related behaviors in youth,” Eating Behaviors 18 (August 2015), 160-78 summarize that, “[t]hirty-four articles, including three intervention studies, were reviewed. The TPB was most often used to evaluate healthy eating and sugary snack and beverage consumption. Attitude had the strongest relationship with dietary behavioral intention (mean r = 0.52), while intention was the most common predictor of behavior performance (mean r = 0.38; both p < 0.001).”
[29] Paul Norman and Mark Conner, “Predicting and changing health behaviour: future directions,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 411.
[30] For example, Jacqueline Panter, Pernille Tanggaard Andersen, Arja R.. Aro, and Anastasia Samara, “Obesity Prevention: A Systematic Review of Setting-Based Interventions from Nordic Countries and the Netherlands,” Journal of Obesity (April 2018), note the lack of SCM theory use: “Several studies (18/33) did not use theory explicitly and others used theories as the basis for choice of study design or approach (3/33). Some of the studies (7/33) built on multicomponent and multilevel interventions such as intervention mapping (IM), socioecological theories or models, and models for individual behaviour; for example, theory of planned behaviour (TPB), social cognitive learning theory (SCT), and health belief model (HBM). Especially in the whole of community and school-based interventions, the background and theoretical frameworks were linked to theories of empowerment, participation, and whole-school participatory tailored approaches (5/33). Across the studies, there existed “a light way” of using theory. Theoretical framework was more often simply referred to, rather than something that was used concretely in problem formulation and as a basic structure in the studies.” The authors therefore conclude that, “[t]here is a need to prioritise interventions that include study designs of high quality [and] the use of theoretical constructs to guide the studies.”
[31] Ryan E. Rhodes, Ian Janssen, Shannon S. D. Bredin, Darren E. R. Warburton, and Adrian Bauman, “Physical activity: Health impact, prevalence, correlates and interventions,” Psychology & Health 32 (May 2017), 22 notes that “Seventeen reviews of adult interventions and four reviews of interventions among young people explored whether the use of theory compared to no reported theory moderated PA change. Among the adult literature, the theories applied most for this evaluation were Bandura’s (1998) social cognitive theory (88% of reviews) and Prochaska and DiClemente’s (1982) Transtheoretical Model (82% of reviews), followed by Ajzen’s (1991) theory of planned behaviour (29% of reviews). No difference in the application of theory on PA outcomes was reported in 76% of reviews, while 18% of the reviews drew the conclusion that the presence of a stated theory was associated with more successful interventions. Among young people, the theoretical applications all involved variants of social cognitive theory and 75% of reviews concluded no difference between use of a reported theory or no such reporting. One review showed that interventions not reporting a theory resulted in greater PA than those based on an explicit theory. Overall, the evidence suggests that explicit use of theory does not moderate the effectiveness of interventions among youth or adults, yet the use of theory thus far is limited to the social cognitive tradition.”
[32] Desmond McEwan, Mark R. Beauchamp, Christina Kouvousis, Christina M. Ray, Anne Wyrough, and Ryan E. Rhodes, “Examining the active ingredients of physical activity interventions underpinned by theory versus no stated theory: A meta-analysis,” Health Psychology (November 2018) found that “There were no significant differences in the overall effect sizes between theory-based (k = 148, d = 0.48) and no-stated-theory (k = 77, d = 0.37) interventions.” However, they did find differences in the use of BCTs between theory-based and no-state-theory interventions and suggest that “for interventions utilizing certain BCT clusters (namely, ‘self-belief’ and ‘association’), theory may be necessary to derive significant effects.”
[33] Eileen F. S. Kaner, Fiona R. Beyer, Claire Garnett, David Crane, Jamie Brown, Colin Muirhead, James Redmore, Amy O'Donnell, James J. Newham, Frank de Vocht, Matthew Hickman, Heather Brown, Gregory Maniatopoulos, and Susan Michie, “Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community‐dwelling populations,” Cochrane Database of Systematic Reviews 9 (September 2017) note that, “[t]he most frequently mentioned theories or models in the included studies were Motivational Interviewing Theory (7/20), Transtheoretical Model (6/20) and Social Norms Theory (6/20). Over half of the interventions (n = 21, 51%) made no mention of theory. Only two studies used theory to select participants or tailor the intervention. There was no evidence of an association between reporting theory use and intervention effectiveness.”
Nicola Black, Barbara Mullan, and Louise Sharpe, “Computer-delivered interventions for reducing alcohol consumption: meta-analysis and meta-regression using behaviour change techniques and theory,” Health Psychology Review 10, no. 3 (2016), 14, note that, “[s]ix theories were tested in their associations with reductions in alcohol consumption.” They found positive outcomes among studies using social norms theory, “however, there was little-to-no evidence that use of the other tested theories – the health belief model, motivational interviewing theory, social cognitive theory, the theory of planned behaviour or the transtheoretical model – improved CDI outcomes, compared to no theory.”
[34] A. Prestwich, F. F. Sniehotta, C. Whittington, S. U. Dombrowski, L. Rogers, and S. Michie, “Does theory influence the effectiveness of health behavior interventions? Meta-analysis,” Health Psychology 33, no. 5 (2014), 465-474. They explain that, “[a]n in-depth analysis of studies included in two systematic reviews of physical activity and healthy eating interventions (k = 190). Extent and type of theory use was assessed using the Theory Coding Scheme (TCS) and intervention effectiveness was calculated using Hedges’s g. Metaregressions assessed the relationships between these measures… Fifty-six percent of interventions reported a theory base. Of these, 90% did not report links between all of their behavior change techniques (BCTs) with specific theoretical constructs and 91% did not report links between all the specified constructs with BCTs. The associations between a composite score or specific items on the TCS and intervention effectiveness were inconsistent.”
[35] Ashleigh A. Armanasco, Yvette D. Miller, Brianna S. Fjeldsoe, and Alison L. Marshall, “Preventive Health Behavior Change Text Message Interventions: A Meta-analysis,” American Journal of Preventive Medicine 52, no. 3 (March 2017), 391-402.
[36] Sarah Browne, Silvia Minozzi, Cristina Bellisario, Mary Rose Sweeney, and Davide Susta, “Effectiveness of interventions aimed at improving dietary behaviours among people at higher risk of or with chronic noncommunicable diseases: an overview of systematic reviews,” European Journal of Clinical Nutrition (October 2018). They add, however, that, “direct associations between theoretical constructs used and dietary outcomes was not established and another review found no association between the use of a theoretical basis and maintenance of dietary change outcomes with the exception of one diet and physical activity study using a combination of TTM/SOC and SCT.” They also add that, “[w]ith the exception of motivational interviewing among patients at high risk of CVD and type 2 diabetes, evidence for the influence of Behavioural Change (BC) theories or techniques on dietary behaviour change was of low quality or absent.”
[37] Cassandra S.Diep Tzu-An Chen, Vanessa F.Davies, Janice C.Baranowski, and Tom Baranowski, “Influence of Behavioral Theory on Fruit and Vegetable Intervention Effectiveness Among Children: A Meta-Analysis,” Journal of Nutrition Education and Behavior 46, no. 6 (December 2014), 506-46. They summarize that, “[d]ifferences in mean Hedges' g effect sizes between theory and non-theory interventions were 0.232 for fruit, 0.043 for vegetables, and 0.333 for fruit and vegetables combined. There was mixed support, however, for enhanced dietary change with multiple theories or a formal planning process. After controlling for study quality, theory use was related only to vegetable consumption (β = 0.373; P < .001).”
[38] Cleo Protogerou and Blair T. Johnson, “Factors Underlying the Success of Behavioral HIV-Prevention Interventions for Adolescents: A Meta-Review,” Aids and Behavior 18, no. 10 (2014).
[39] Olawale Olanrewaju, Sarah Kelly, Andy Cowan, Carol Brayne, and Louise Lafortune, “Physical Activity in Community Dwelling Older People: A Systematic Review of Reviews of Interventions and Context,” PLoS ONE 11, no. 12 (December 2016). One of these was a meta-analysis, which reported SMD 0.14, 95% CI 0.09 to 0.2, p < 0.001.
[40] Kevin A. Cradock, Gearóid ÓLaighin, Francis M. Finucane, Rhyann McKay, Leo R. Quinlan, Kathleen A. Martin Ginis, and Heather L. Gainforth, “Diet Behavior Change Techniques in Type 2 Diabetes: A Systematic Review and Meta-analysis,” Diabetes Care 40, no. 12 (December 2017), 1800-1810. They add that, “[s]imilar findings have been reported, in which dietary behavior interventions in cancer prevention were more effective when informed by theory. However, fidelity of the use of theory was not reported in the studies included in our review or other reviews, and descriptions of use of theory varied considerably from ‘integrated concepts from different theories’ to ‘behavior modification treatment used principles from the modern learning theory’ and ‘group educational classes were based on the social cognitive theory.’ The social cognitive theory was the only theory reported more than once.”
This review was ranked as warranting only “critically low” confidence through AMSTAR 2, but is superior in many ways to many other included reviews.
[41] Keegan Knittle, Johanna Nurmi, Rik Crutzen, Nelli Hankonen, Marguerite Beattie, and Stephan U. Dombrowski, “How can interventions increase motivation for physical activity? A systematic review and meta-analysis,” Health Psychology Review 12, no. 3 (February 2018), 13. They add that, “[t]his finding extends those of previous meta-analyses, which had found that Internet-based interventions based on the theory of planned behaviour had greater effects than other interventions (Webb et al., 2010), and that interventions explicitly based on social-cognitive theory significantly increase physical activity among cancer survivors (Stacey, James, Chapman, Courneya, & Lubans, 2015). Given the important theoretical position of self-efficacy cognitions within both social-cognitive theory and the theory of planned behaviour, and the well-defined direct links between self-efficacy and behaviour in multiple domains, our results confirm the importance of fostering cognitions related to personal control over behaviour in influencing both motivation and physical activity behaviour.”
[42] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 19-20: “First, models that have been developed specifically to predict health behaviour (i.e. health action process approach, health belief model, protection motivation theory) focus on the notion of threat as measured by perceived susceptibility/vulnerability and perceived severity… Second, most social cognition models of health behaviour focus on the perceived consequences of performing a health behaviour… Third, there is considerable overlap between the perceived behavioural control component of the TPB and self-efficacy… Fourth, social cognition models of health behaviour do not explicitly cover normative influences on behaviour (Conner and Norman 1994), with the exception of the TPB, which includes the subjective norm construct and underlying normative beliefs, and the PWM, which also includes the prototype construct… Fifth, nearly all models include an intervening variable that is seen to mediate the relationship between other social cognitive variables and behaviour… Sixth, the TPB, SCT, and HAPA all postulate a direct relationship between self-efficacy (or perceived behavioural control) and behaviour in addition to the one between intention and behaviour… Finally, there are a number of similarities in more recent models (e.g. HAPA) that have sought to outline the variables that are important in the volitional phase of health behaviour (e.g. Weinstein 1988; Heckhausen 1991; Bagozzi 1992; Schwarzer 1992; Gollwitzer 1993; Kuhl and Beckmann 1994). In particular, these models emphasize the need for individuals to deploy a range of self-regulatory skills and strategies to ensure that strong intentions are translated into behaviour.”
[43] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 21 note that, “[m]ost prominent among these attempts is the work of a number of major theorists who attended a workshop organized by the National Institute of Mental Health in response to the need to promote HIV-preventive behaviours… who sought to ‘identify a finite set of variables to be considered in any behavioural analysis’ (Fishbein et al. 2001: 3). They identified eight variables, which, they argued, should account for most of the variance in any (deliberative) behaviour (Figure 1.1). These were organized into two sets. The first set were those variables that they viewed as necessary and sufficient determinants of behaviour. Thus, for behaviour to occur, an individual must (i) have a strong intention, (ii) have the necessary skills to perform the behaviour, and (iii) experience an absence of environmental constraints that could prevent behaviour. The variables in the second set were primarily seen to influence intention, though it was noted that some of the variables may also have a direct effect on behaviour. Thus, a strong intention is likely to occur when an individual (iv) perceives the advantages (or benefits) of performing the behaviour to outweigh the perceived disadvantages (or costs), (v) perceives the social (normative) pressure to perform the behaviour to be greater than that not to perform the behaviour, (vi) believes that the behaviour is consistent with his or her self-image, (vii) anticipates the emotional reaction to performing the behaviour to be more positive than negative, and (viii) has high levels of self-efficacy.”
[44] Mark Conner and Paul Norman, “Predicting and changing health behaviour: a social cognition approach,” in Mark Conner and Paul Norman (eds.), Predicting and changing health behaviour: Research and practice with social cognition models (Maidenhead: Open University Press, 2015; first published 1995), 22 criticize Fishbein et al’s 2001 combined model: “First, it includes a number of constructs that do not feature in the main social cognition models… Second, it is noteworthy that the integrated model fails to include perceptions of susceptibility and severity, which are key constructs in the health belief model and protection motivation theory… Third, the model lacks detail regarding the relationships between its constructs. In fact, Fishbein et al. (2001) noted that the major theorists were unable to agree on the likely nature of these relationships… Fourth, no empirical test of the model has been conducted to date... Finally, the model is fairly mute on the post-intentional (i.e. volitional) phase of health behaviour, simply stating that in addition to a strong intention, an individual must also possess the necessary skills to perform the behaviour and not encounter any environmental constraints that could prevent performance of the behaviour.”